Radiologists are understandably nervous about the Medicare rule requiring the use of Appropriate Use Criteria and Clinical Decision Support (AUC/CDS) systems.
HAP USA
Recent Posts
Radiologists on Appropriate Use Criteria Support | HAP on May 8, 2017
Categories: radiology reimbursement, radiology documentation, clinical decision support, CDS
Proper Use of Medicare ABN's for Radiology Practices on May 1, 2017
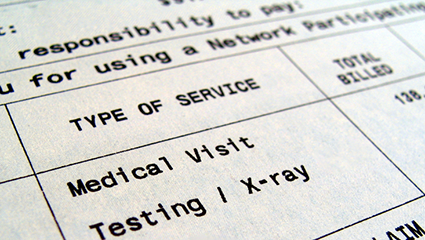
There are circumstances where payment is expected to be denied by Medicare for radiology services to be provided to a Medicare patient. In such cases, the radiology practice must look to the patient for payment. However, without following proper procedures the practice will be precluded from collecting from either the patient or Medicare.
Categories: radiology reimbursement, medicare reimbursement
The Need for Standardized Radiology Documentation to Maximize Medicare Reimbursements on March 10, 2017
Accuracy and completeness in radiology reporting has taken on an even higher level of importance in order to maximize Medicare reimbursement. The Quality Payment Program (QPP) under MACRA highlights the necessity to meet new quality performance standards. While the benefits of structured reporting using templates have been discussed before, including in our article Reimbursement Benefits of Structured Radiology Reporting, reporting on quality measures under the QPP has to include very specific terminology in order to receive credit for the measure. This is an ideal time for radiologists to begin to use standardized reporting across their practice to ensure that all of the critical elements of documentation are met.
Categories: radiology reimbursement, medicare reimbursement, MIPS, MACRA
How to Be Sure Your Radiology Documentation Supports Proper Coding for Moderate Sedation on March 2, 2017
While certain procedures incorporate moderate sedation (also known as conscious sedation) into their treatment codes, according to modern CPT® guidelines, it is much more common to bill procedures and anesthetics separately. This enables greater specificity in billing regarding time spent and provider involvement. As a radiology practice, maintaining moderate sedation billing compliance is crucial to your financial wellness and practice reputation. Whether you are new to billing and coding or need a refresher, Healthcare Administrative Partners' expertise is here to help.
Understanding Moderate Sedation Coding for Radiology
Previous coding methodology allowed for billing in 15- and 30-minute increments and included code series 99143-99145 and 99148-99150. However, these features became obsolete in 2017. The new standard of radiology moderate sedation documentation includes codes 99151-99153 and 99155-99157, and is based on factors of:
- 15-minute intervals: Intraservice time must be recorded in minutes. You may report the initial 15-minute code once you document at least 10 minutes of intraservice time. Then, you may report each additional 15-minute add-on code once you have provided at least 8 minutes beyond the first 15 minutes.
- Physicians involved: The proper code will vary depending on whether the administering physician is the same physician performing the diagnostic or therapeutic service or a separate person.
- Patient age: There are separate codes for patients under 5 years of age and those 5 or older.
These tables should help you understand which codes apply to which services.
[On-site table 1 - Descriptors]
[On-site table 2 - Total intraservice time]
*Note that for Medicare, 99153 is a technical-only add-on code in facility settings. It is packaged into the facility payment and is not separately reimbursed to the physician — physicians are only paid for 99151 and 99152 codes.
How to Document Moderate Sedation Properly
With all this information in mind, every moderate sedation record should provide these key pieces of data:
- Patient age
- Physician(s) name(s)
- Physician or physician's clinical need for participation
- Intraservice time (total time in minutes and start/end time stamps)
- The term “moderate” or “conscious” sedation
- Any pre- or post-sedation monitoring and assessments
- Pre- and post-sedation work the physician performs
Here is an example of good documentation for moderate sedation:
Moderate intravenous conscious sedation was supervised by Dr. X. The patient was independently monitored by a Registered Nurse assigned to the Department of Radiology using automated blood pressure, EKG and pulse oximetry. The detailed Conscious Record is permanently stored in the Hospital Information System. The following is the conscious sedation record including Start and End times: MEDS GIVEN 4 MG VERSED AND 200 MCG FENTANYL; SED START 1503 END 1531, FOR 28 MINUTES.
Stay Informed and Supported at HAP USA
Proper coding allows radiology practices like yours to obtain the maximum reimbursement for the services you offer, promoting long-term financial integrity that allows you to continue serving patients in need. Healthcare Administrative Partners is dedicated to helping providers optimize their performance with expert revenue cycle management advice and solutions. Stay up to date on the latest industry news when you subscribe to our blog. Or, contact us directly to learn more about how we can actively support your operations.
Categories: radiology documentation, radiology coding
Assessing the Impact of High Deductible Health Plans on Radiology Practices on February 16, 2017
Before the days of managed care, insurance plans were “indemnity coverage” that reimbursed patients for their out-of-pocket costs. Physicians billed the patients and got paid when the patients felt like making payment, usually only after the insurance company had reimbursed them. Often, the insurance money went elsewhere in the patient’s budget and the physician waited for payment. The not-so-good old days! With the advent of managed care contracting where physicians were paid directly by the insurance company, patient balance collections mostly disappeared. Today the pendulum is swinging back in the opposite direction, requiring practices to once again face the necessity to collect significant balances from patients.
Categories: radiology reimbursement, radiology billing
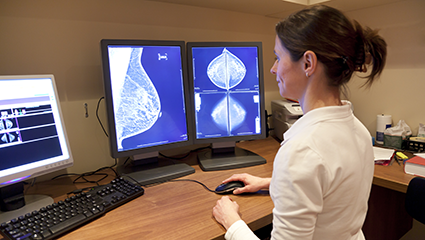
Maximize Mammography Coding and Billing Efficiency in 2017 on January 28, 2017
Medicare publishes its rules and requirements for the coding and billing of medical procedures to obtain reimbursement under its programs, but many commercial insurers are not as transparent about their own requirements. This leaves medical billing professionals in the dark when there are new procedure codes or changes to existing coding in the American Medical Association’s CPT® code set or by federal regulation. Such is the case with mammography coding for 2017. Below we have summarized the key coding considerations for radiology practices billing mammography services this year. (Click here to read our complete article on the 2017 coding changes impacting diagnostic and intervential radiology.)
Categories: radiology reimbursement, radiology coding, breast imaging
2017 Interventional Radiology CPT Codes Update | HAP USA on January 27, 2017
Click here to read our 2024 code changes update article.
The annual cycle of revising codes in the Current Procedural Terminology (CPT)® has been completed with the issuance of the Medicare Physician Fee Schedule (MPFS) Final Rule for 2017. For diagnostic radiology, the changes this year are in mammography bundling, ultrasound screening for abdominal aortic aneurysm, and fluoroscopic guidance. Interventional Radiology (IR) will also be subject to bundling and other rearranging of codes for certain procedures. Finally, there are new codes that have been created to describe procedures previously unlisted, which generally will improve reimbursement for those procedures, and codes deleted from use, which will return the affected procedures to the ‘unlisted’ category.
Categories: radiology reimbursement, radiology coding, interventional radiology, IR coding, CPT codes
Regulatory Changes Affecting Radiology Reimbursement in 2017 on December 10, 2016
Looking for our latest article on the 2018 updates? Click here.
Congress has passed several Acts related to the Medicare payment system over recent years, the provisions of which will begin to take effect in 2017. These changes are embodied in the annual Medicare Physician Fee Schedule Final Rule for 2017 (MPFS) and the Hospital Outpatient Prospective Payment System Final Rule for 2017 (HOPPS). In their initial review of the MPFS, the American College of Radiology (ACR) indicated that it “is pleased with several provisions within the rule.”
Categories: radiology reimbursement
Finalized MACRA Rules for 2017 Contain Some Good News for Radiologists on October 22, 2016
Earlier this year CMS published its proposed regulations that would implement the MACRA law to revamp the Medicare physician payment system. On October 14th, after consideration of over 4,000 comments about the proposed rules, CMS published the final rule that will govern the initial measurement period that begins January 1, 2017 for payment adjustments in 2019.
Categories: radiology reimbursement, MIPS, MACRA, Quality Payment Program
What Radiology Practices Need to Know About the 2017 MPPR Update on October 13, 2016
Since its first appearance in the Medicare rules, the radiology community has been quarreling with CMS about the Multiple Procedure Payment Reduction (MPPR) on the professional component of certain diagnostic imaging services. Finally, Congress has taken steps to mitigate the impact of this rule.
Categories: radiology reimbursement, mppr