 There are circumstances where payment is expected to be denied by Medicare for radiology services to be provided to a Medicare patient. In such cases, the radiology practice must look to the patient for payment. However, without following proper procedures the practice will be precluded from collecting from either the patient or Medicare.
There are circumstances where payment is expected to be denied by Medicare for radiology services to be provided to a Medicare patient. In such cases, the radiology practice must look to the patient for payment. However, without following proper procedures the practice will be precluded from collecting from either the patient or Medicare.
When patients are expected to become financially responsible for payment they must be advised in advance, with enough opportunity for them to consider their options. Practices should be using a form known as an Advance Beneficiary Notice of Noncoverage (ABN) to notify patients of the circumstances under which they will be responsible for payment, and to obtain their consent to assume responsibility.
Practices may choose to use either the form that is issued by Medicare for this purpose, or one created by the practice provided that it includes certain information prescribed by the federal regulations. Medicare recently revised their standard ABN Form (CMS-R-131) in March 2017, as they do every three years.
ABNs are most often used in radiology practices when:
- Medicare usually covers a procedure but it is being performed more frequently than the Medicare coverage guidelines allow. Examples include screening mammograms or CT colorectal cancer screenings, which will be denied if they are performed more frequently than the Medicare coverage guidelines allow. If patients wish to receive such services more frequently than the allowed timeframe, they must sign an ABN before the procedure is performed to acknowledge that they will be responsible for payment.
- Medicare does not cover a procedure ordered by a physician for the patient’s particular diagnosis.
Some procedures are subject to Local Coverage Determinations (LCD) rather than national policy. If the service does not meet the requirements for medical necessity, then the use of an ABN is recommended. Some examples of radiology procedures in this category include:
- 3D interpretation and reporting of imaging studies
- Barium Swallow studies
- Magnetic Resonance Angiography (MRA)
- Non-invasive peripheral venous studies
- Non-vascular extremity ultrasound
Note that an ABN is not required for services that are never covered by Medicare (non-covered services). In these cases, practices might want to use the form as a courtesy to notify the patient of his or her financial responsibility. This will avoid any misunderstanding and assist in collecting payment from the patient.
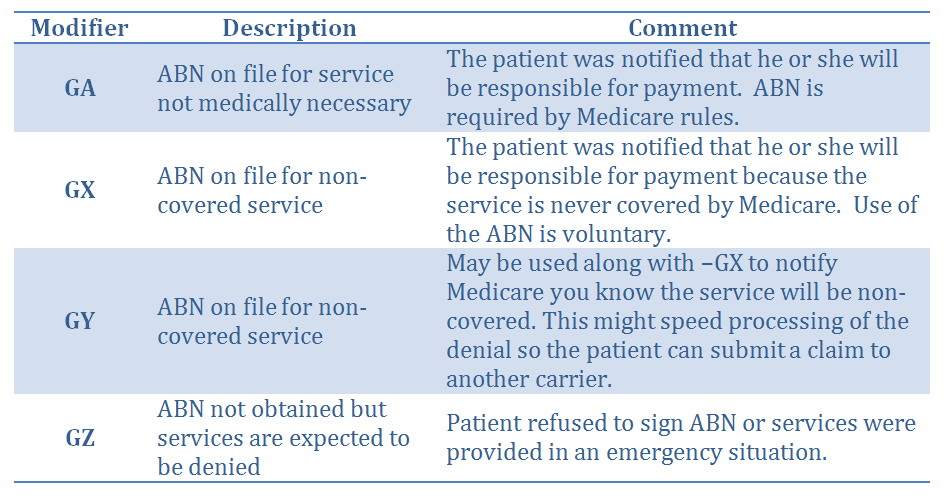
Billing modifiers are used to notify Medicare of the existence of the ABN, as follows:
The practice will not be able to legally collect its fee from the patient unless it obtained the patient’s consent on an ABN form signed before the procedure is performed. Routine ABNs that are issued without any reason to believe Medicare will not pay for the service are not allowed. An ABN must be issued only when there is a specific reason to believe Medicare will deny payment for the service, and the form must list the specific procedure and the reason Medicare might not pay for it. More than one procedure can be listed on a single form, when applicable.
Proper use of Advance Beneficiary Notice of Noncoverage (ABN) forms is an important part of maintaining both the practice’s revenue stream and patient relationships. When used properly, patients may be billed for service payments denied by Medicare. ABNs also inform patients in advance that they will have to pay for those services, which will aid in the collection of fees. Practices should be sure to review their forms periodically, and update any non-standard forms to conform to current regulations. The latest version of the ABN form must be in use by June 21, 2017.
Related articles:
The Need for Standardized Radiology Documentation to Maximize Medicare Reimbursements
One Simple Way a Radiology Group Added Value to Their Hospital Relationship



