While certain procedures incorporate moderate sedation (also known as conscious sedation) into their treatment codes, according to modern CPT® guidelines, it is much more common to bill procedures and anesthetics separately. This enables greater specificity in billing regarding time spent and provider involvement. As a radiology practice, maintaining moderate sedation billing compliance is crucial to your financial wellness and practice reputation. Whether you are new to billing and coding or need a refresher, Healthcare Administrative Partners' expertise is here to help.
Understanding Moderate Sedation Coding for Radiology
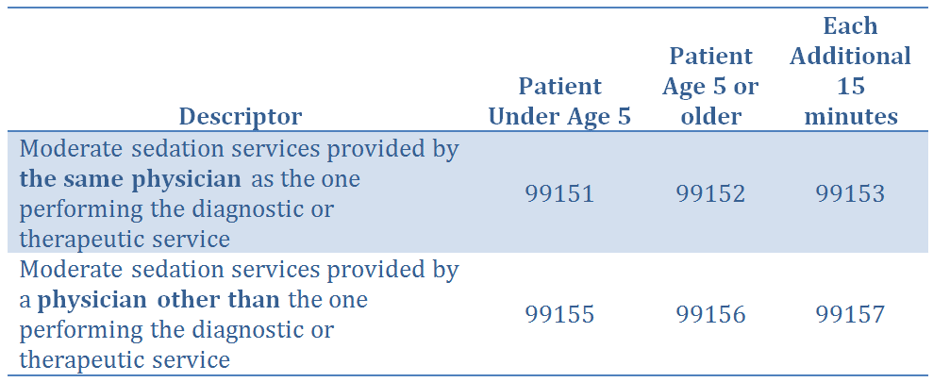
Previous coding methodology allowed for billing in 15- and 30-minute increments and included code series 99143-99145 and 99148-99150. However, these features became obsolete in 2017. The new standard of radiology moderate sedation documentation includes codes 99151-99153 and 99155-99157, and is based on factors of:
- 15-minute intervals: Intraservice time must be recorded in minutes. You may report the initial 15-minute code once you document at least 10 minutes of intraservice time. Then, you may report each additional 15-minute add-on code once you have provided at least 8 minutes beyond the first 15 minutes.
- Physicians involved: The proper code will vary depending on whether the administering physician is the same physician performing the diagnostic or therapeutic service or a separate person.
- Patient age: There are separate codes for patients under 5 years of age and those 5 or older.
These tables should help you understand which codes apply to which services.
[On-site table 1 - Descriptors]
[On-site table 2 - Total intraservice time]
*Note that for Medicare, 99153 is a technical-only add-on code in facility settings. It is packaged into the facility payment and is not separately reimbursed to the physician — physicians are only paid for 99151 and 99152 codes.
How to Document Moderate Sedation Properly
With all this information in mind, every moderate sedation record should provide these key pieces of data:
- Patient age
- Physician(s) name(s)
- Physician or physician's clinical need for participation
- Intraservice time (total time in minutes and start/end time stamps)
- The term “moderate” or “conscious” sedation
- Any pre- or post-sedation monitoring and assessments
- Pre- and post-sedation work the physician performs
Here is an example of good documentation for moderate sedation:
Moderate intravenous conscious sedation was supervised by Dr. X. The patient was independently monitored by a Registered Nurse assigned to the Department of Radiology using automated blood pressure, EKG and pulse oximetry. The detailed Conscious Record is permanently stored in the Hospital Information System. The following is the conscious sedation record including Start and End times: MEDS GIVEN 4 MG VERSED AND 200 MCG FENTANYL; SED START 1503 END 1531, FOR 28 MINUTES.
Stay Informed and Supported at HAP USA
Proper coding allows radiology practices like yours to obtain the maximum reimbursement for the services you offer, promoting long-term financial integrity that allows you to continue serving patients in need. Healthcare Administrative Partners is dedicated to helping providers optimize their performance with expert revenue cycle management advice and solutions. Stay up to date on the latest industry news when you subscribe to our blog. Or, contact us directly to learn more about how we can actively support your operations.
New Coding Structure Using Intraservice Time and Patient Age
The new series of codes describe moderate sedation services in 15-minute increments. This replaces the previous series that included both 30- and 15-minute increments. The codes are now differentiated by the age of the patient (under age 5 vs. age 5 or above) and whether performed by the same physician as the one who is performing the primary procedure or by a different physician.
These new codes need to be reported separately in conjunction with the primary procedure in order for the radiology practice to be fully reimbursed for all services rendered:
The old code series 99143-99145 and 99148-99150 have been eliminated. Reimbursement will be reduced for those procedures that previously included moderate sedation as a bundled service, now that the sedation will be billed and paid separately.
The new codes are based on intraservice time, which must be clearly documented. Intraservice time begins with the administration of the sedating agent and it requires continuous face-to-face attention by the physician. It ends when the procedure is completed, the patient is stable, and the physician providing the sedation feels comfortable leaving the face-to-face care of the patient.
The primary codes for the appropriate age grouping are used for the initial 15 minutes of intraservice time, and the add-on codes are used for each additional 15-minute interval. The documentation should include the full range of intraservice time, although intervals of less than 10 minutes should not be billed for. The following table can be used as a guide under the new coding structure:
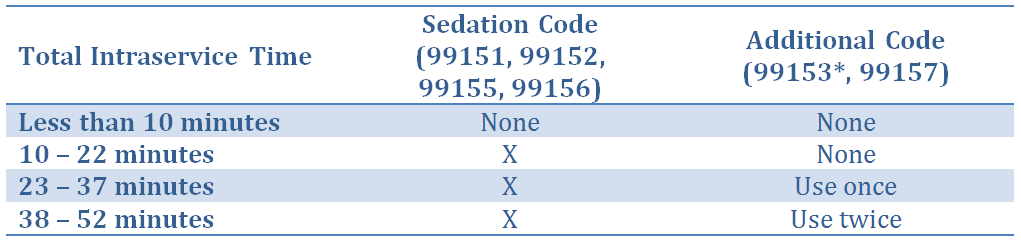
* Note that 99153 is designated by Medicare as a “technical-only” code when services are performed in a facility such as a hospital. This means that it is not to be used by the same physician as the one performing the procedure in such a location, whether the services are for inpatients or outpatients. The result is that Medicare will not reimburse any intraservice time over the initial 15 minutes. However, for patients in an office setting the code should be allowed.
Other payers are treating code 99153 differently than Medicare does, and HAP recommends that practices continue to record and bill for all of the intraservice time involved in procedures. In the event Medicare changes its position, the data will be readily available so that prior claims can be appealed for payment.
Documentation Requirements
The coding of moderate sedation is based on three key elements, all of which must be clearly stated in the operative report:
- the patient’s age
- the intraservice time
- the physician who provided the sedation
The beginning and ending intraservice times can be reported, but including the elapsed length of time in minutes will make the coder’s job easier and it will also facilitate any subsequent compliance or post-payment reviews. Including the terms “moderate” or “conscious” sedation will leave no doubt as to the service that was performed. In addition, any pre- or post-sedation assessment or monitoring should be reported. When a separate physician provides sedation, the clinical reason for his or her participation should be documented, along with any pre- or post-service work performed.
Here is an example of good documentation for moderate sedation:
Moderate intravenous conscious sedation was supervised by Dr. X. The patient was independently monitored by a Registered Nurse assigned to the Department of Radiology using automated blood pressure, EKG and pulse oximetry. The detailed Conscious Record is permanently stored in the Hospital Information System. The following is the conscious sedation record including Start and End times: MEDS GIVEN 4 MG VERSED AND 200 MCG FENTANYL; SED START 1503 END 1531, FOR 28 MINUTES.
Summary
Radiology practices must review their historical billing to determine if they perform procedures that previously bundled moderate sedation into the primary procedure code. When these procedures are done, the new separate sedation codes are used. Radiologists performing these procedures must document the critical elements for proper coding, in addition to their normal procedural description, in order to prevent lost practice reimbursement.
Subscribe to our blog or contact Healthcare Administrative Partners for more information.
[i] Current Procedural Terminology is a copyrighted code set developed and maintained by the American Medical Association, and CPT is a registered trademark.
This article was updated on June 7, 2017.
Related articles:
How the 2017 Coding Changes Will Affect Diagnostic and Interventional Radiology Practices
Maximize Mammography Coding and Billing Efficiency in 2017