Read our 2021 IR billing & coding article
A radiology practice that performs interventional procedures will want to be up to date on the use of documentation and coding techniques for Evaluation and Management (E&M) services. These CPT® codes in the 99xxx range are less commonly utilized in radiology practices. Identifying circumstances where E&M services are billable, and then properly documenting and coding for them, will require a collaborative effort between the interventional radiologist (IR) and his or her coding team.
Categories:
radiology billing,
radiology coding,
interventional radiology,
radiology
Radiologists considering the use of an outside service for final reads will have questions that include not only quality and cost but also the impact on the group’s relationship with its hospital and referring physician community. The answer will not be the same for every radiology practice. Here we present some of the pros and cons for consideration in the decision-making process.
Categories:
radiology billing,
radiology,
teleradiology billing,
teleradiology
Maximizing the patient experience is no longer limited to the achievement of clinical success. It is a critical component of the new, broader partnership between provider and patient – one that now encompasses conversations regarding not only service quality and cost, but also places a greater focus on practice billing processes in line with the higher demands inherent to the new patient consumerism trend.
Categories:
radiology reimbursement,
radiology billing,
patient collections
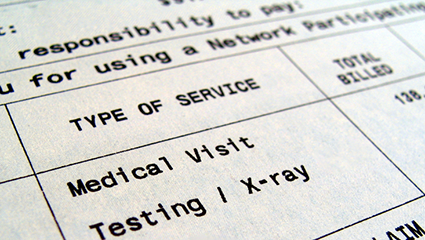
Before the days of managed care, insurance plans were “indemnity coverage” that reimbursed patients for their out-of-pocket costs. Physicians billed the patients and got paid when the patients felt like making payment, usually only after the insurance company had reimbursed them. Often, the insurance money went elsewhere in the patient’s budget and the physician waited for payment. The not-so-good old days! With the advent of managed care contracting where physicians were paid directly by the insurance company, patient balance collections mostly disappeared. Today the pendulum is swinging back in the opposite direction, requiring practices to once again face the necessity to collect significant balances from patients.
Categories:
radiology reimbursement,
radiology billing
If you follow the leading voices in the radiology community, you know that the topic of “value” is a recurring theme of current conversations. It is a core concept behind Imaging 3.0 and has dominated recent seminars, webinars, social media chatter and more for months thanks to MACRA and the many changes it is bringing to provider compensation models. And whatever changes the next wave of governmental healthcare policy washes into the boardrooms of group practices, when the murky waters recede, it is a safe bet that proof-of-value will still remain on the table as a mandate for radiologists going forward.
Categories:
radiology billing,
radiology value building
Our first article in this series provided a list of questions to ask when evaluating a professional services Revenue Cycle Management (RCM) vendor for your radiology practice. If your current RCM vendor cannot answer all of them positively, it’s time to look for a new vendor. With a large number of RCM companies available in the market, how should you decide which one to choose?
Categories:
radiology reimbursement,
radiology billing,
radiology coding
When a major hospital-based radiology practice realized that their outpatient volume had dropped suddenly, their Revenue Cycle Management (RCM) company stepped up to quickly diagnose the problem. Using their analytic database, they produced a focused referring doctor report that revealed significant outpatient service volume declines concentrated among a handful of providers, one of which had decreased by 60%. It’s this kind of responsiveness that sets a true RCM partner apart from the average vendor.
Categories:
radiology billing,
radiology coding

Interventional Radiology Meets Radiation Oncology – The y-90 Story
When a physician is performing an interventional procedure valued in the range of $4,000 – $6,000 for the professional component, attention to thorough and accurate documentation is a requirement for maximal reimbursement. Each case presents its own individual set of circumstances and a well-constructed operative report will tell the story of the case step-by-step. Each artery or branch into which a catheter is placed for diagnostic imaging or intervention is assigned a separate CPT code, and so the operative report must describe with specificity each catheter placement. When these descriptions are in a logical, sequential order, certified coders say that this allows them to better understand every aspect of the case so they can then accurately identify and apply up to 45 CPT codes to maximize reimbursement for it. A descriptive evaluation of each artery supports payment of the codes that are submitted for reimbursement.
Categories:
radiology reimbursement,
radiology billing,
physician reimbursement,
radioembolization,
interventional radiology,
nuclear medicine,
y-90
Four new HCPCS modifiers will be available for use beginning in 2015, according to a recent announcement by the Centers for Medicare and Medicaid Services (CMS). Known collectively as the –X{EPSU} Modifiers, they will be used to define specific subsets of the CPT Modifier -59 for a “Distinct Procedural Service”. The new modifiers are intended to offer more precise coding options that will allow practices to avoid potential payment delays, audits and reviews associated with modifier -59. CMS says that -59 is the most widely used modifier, covering a wide variety of circumstances such as to identify different encounters, different anatomic sites and distinct services. Because modifier -59 is so broadly defined, it is often used incorrectly and inappropriately.
Categories:
radiology billing,
medicare,
radiology coding,
medicare reimbursement,
modifier -59,
mppr,
X{EPSU} Modifiers,
cms
When the dust finally settled, we could see how the 2014 Medicare Physician Fee Schedule (MPFS) would impact radiology reimbursement, and results were mixed. Hospital-based services came out ahead while imaging centers generally took a big hit. Due to the many factors that contribute to the calculation of the final fee schedule, a weighted analysis will help you determine the actual impact on your practice.
Categories:
radiology reimbursement,
radiology billing,
regulatory,
medicare reimbursement