The Medicare Physician Fee Schedule (MPFS) Final Rule for 2022 contained a 3.71% decrease in the Conversion Factor (CF), as we reported in our recent review of the rule. However, after lobbying by physicians and their representative organizations, Congress passed the Protecting Medicare and American Farmers from Sequester Cuts Act (the Act) that rolls back most of that cut and boosts the fee schedule that was contained in the MPFS Final Rule by 3%. We calculate that the CF for 2022 will therefore be $34.6062 instead of $33.5983, although the exact figure has not yet been released.
Congress Responds to Lessen Medicare Cuts For 2022 on December 17, 2021
Categories: medicare, medicare reimbursement, Medicare Physician Fee Schedule
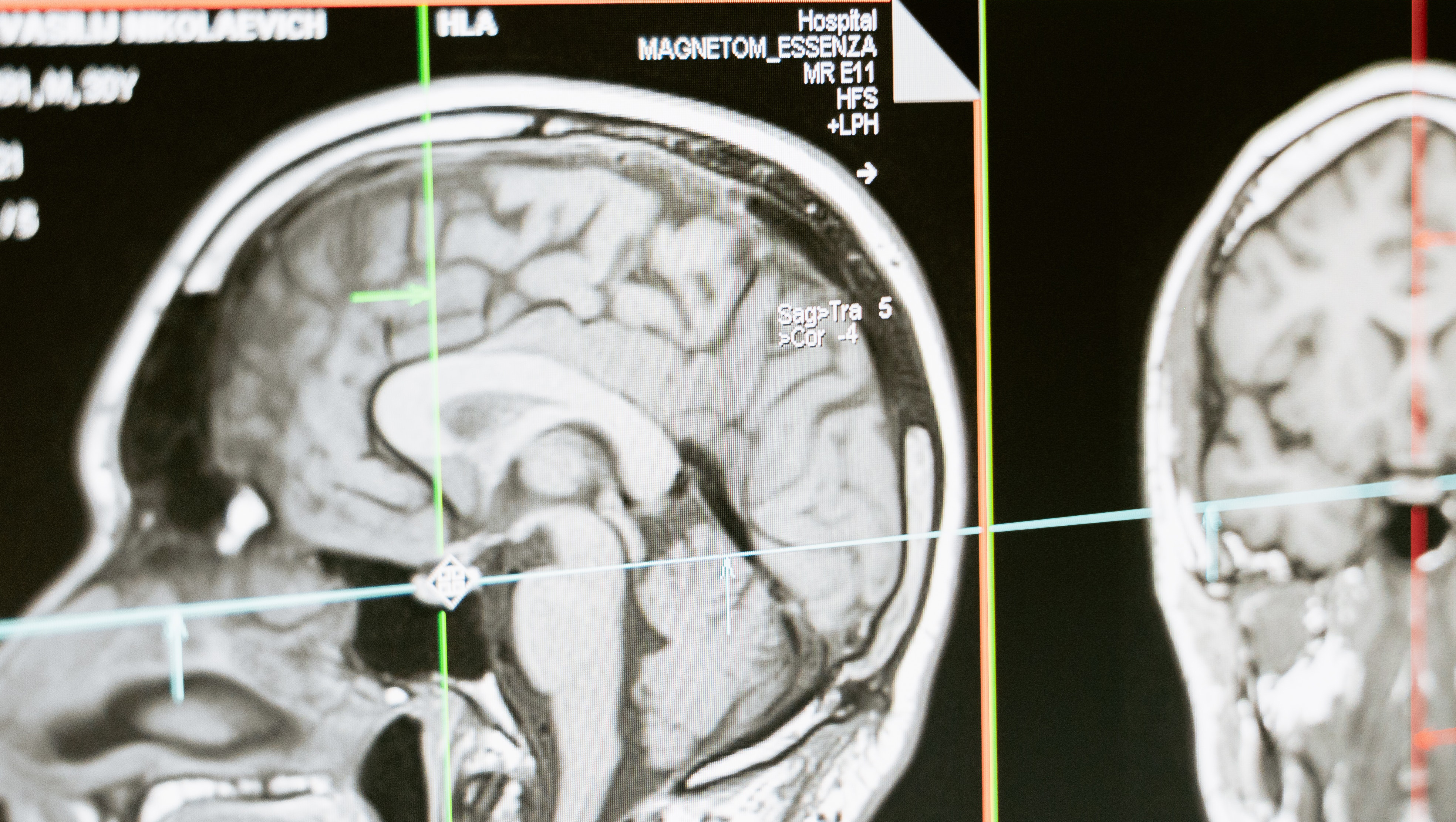
More Evidence That Radiology is Not the Source of Medicare Spending Increases on September 22, 2021
It seems that diagnostic imaging and radiology are often blamed for increasing the cost of healthcare, especially Medicare costs. Not so, says a recent study that was reported in Radiology Business on August 30, 2021.
An Important Deadline for Radiology Practices to Comply with the Medicare AUC/CDS Mandate on June 16, 2021
On January 1, 2022, radiology practices and hospitals that perform certain imaging services for Medicare patients will be denied payment for those services unless they submit documentation that the ordering physician has consulted a Clinical Decision Support (CDS) system. This regulation was included a few years ago in Medicare rulemaking, but its effective date has been delayed several times. As of now, there is no reason to believe it will be postponed further, so practices that have not yet taken steps to install and implement a system have a narrow window of opportunity to get ready.
Categories: medicare, medicare reimbursement, nuclear medicine, CT imaging, MRI, CDS, radiology, AUC, referring physicians, PET, 2022 payment impact
Federal Programs to Assist Radiology Practices During the Pandemic on March 30, 2021
At around this time last year we were beginning to learn about the various ways medical practices could make use of federal programs to help keep them afloat through the COVID-19 pandemic. No one knew how long it would last. As time went on, we followed the changes to those programs, the new programs that became available, and the deadlines for action. Let’s review the latest federal legislation and also where each of last year’s relief programs stands today, especially the Medicare Payment Sequester that is a developing story.
Categories: medicare, radiology, teleradiology, PPP
Understanding the Impact of The Medicare Fee Schedule for 2021 on Your Radiology Practice on January 25, 2021
When the Medicare Physician Fee Schedule (MPFS) Final Rule was published in December, it looked like radiology was facing a significant cut in Medicare reimbursement for 2021. Our article reported that professional component fees would drop 10-11% while global reimbursement would see a lesser impact. The Consolidated Appropriations Act, 2021 (CAA) rolled back those cuts at least for 2021, although the Medicare fee schedule for radiology will likely continue to be adjusted downward in the future as implementation of the revalued Evaluation and Management (E&M) services is fully phased in.
Categories: radiology reimbursement, medicare, medicare reimbursement, MPFS, radiology
How the Consolidated Appropriations Act Will Impact Radiology Practices on January 18, 2021
The “Consolidated Appropriations Act, 2021” (CAA) is a sweeping piece of legislation that provides relief to individuals and businesses impacted by the COVID-19 public health emergency. Some of the relief provisions apply to all businesses, including medical practices, but it also contains several measures that specifically apply to medical practices.
Categories: radiology reimbursement, medicare, medicare reimbursement, radiology, surprise billing, Paycheck Protection Program
Medicare Delays Recoupment of Advances on September 10, 2020
One of the fastest and easiest sources of emergency funding available to practices at the outset of the COVID-19 pandemic was the Medicare Accelerated and Advanced Payment Program. As we recently reported, the initial timetable called for repayment of those advances to begin 120 days after the advance was made. Repayment was to be accomplished through reduction of Medicare reimbursements otherwise payable to the practice currently, until the full amount of the advance was repaid.
Categories: medicare, medicare reimbursement, cms, radiology, COVID-19
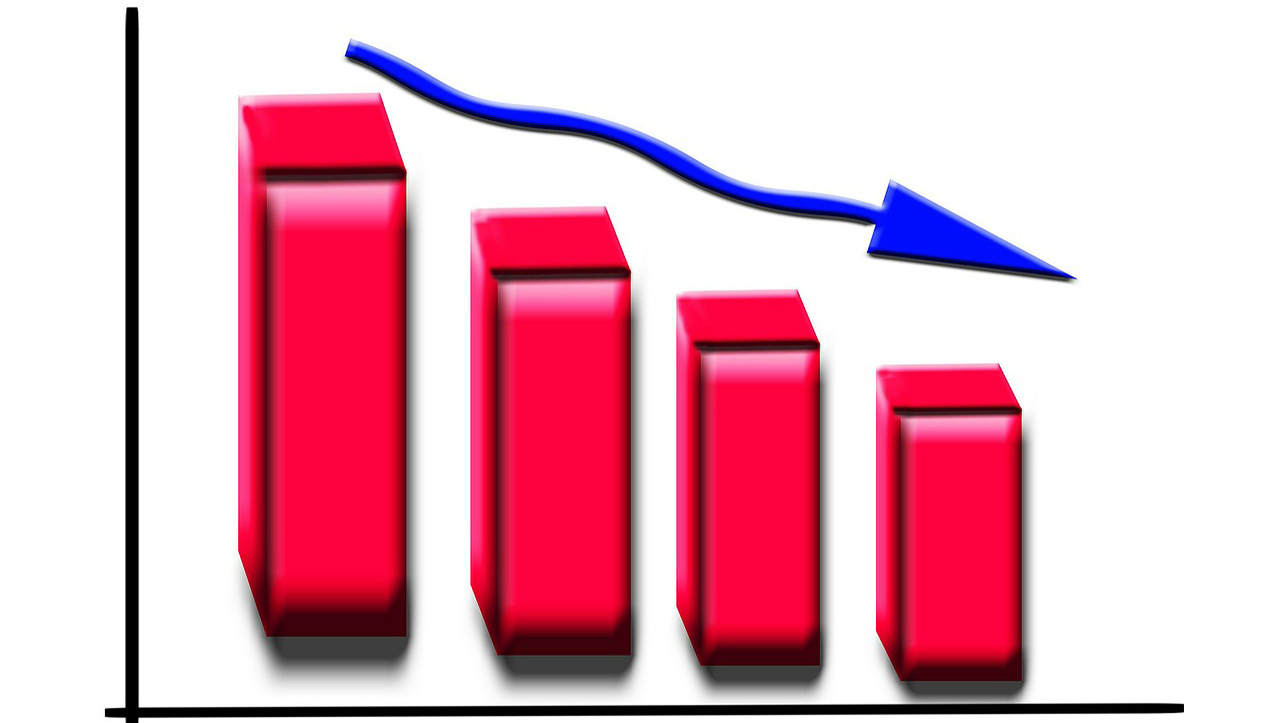
Radiology’s Declining Reimbursement Spans More Than A Decade on August 20, 2020
The average cut of 11% in radiology reimbursement that is proposed by the Medicare Physician Fee Schedule for 2021 (MPFS) is the continuation of a trend that spans more than a decade.
Categories: radiology reimbursement, medicare, medicare reimbursement, MPFS, radiology
Medicare Proposed Major Cut in Radiology Reimbursement for 2021 on August 14, 2020
The Centers for Medicare and Medicaid Services (CMS) has released their annual proposal for changes to the Medicare payment system for the coming year. The Medicare Physician Fee Schedule (MPFS) Proposed Rule contains not only proposed adjustments to Medicare reimbursement but also proposed changes to the Quality Payment Program (QPP) for 2021 and beyond.
Categories: radiology reimbursement, medicare, medicare reimbursement, cms, radiology
Early Pandemic Funding Sources May Require Action Now on July 30, 2020
Much has been written about the Paycheck Protection Program (PPP) loans and the complex rules for loan forgiveness, but there were other funding sources available early in the public health emergency that need to be revisited now. Our article in April outlined the HHS Grant Funds and another article discussed the Medicare Accelerated & Advance Payments Program.