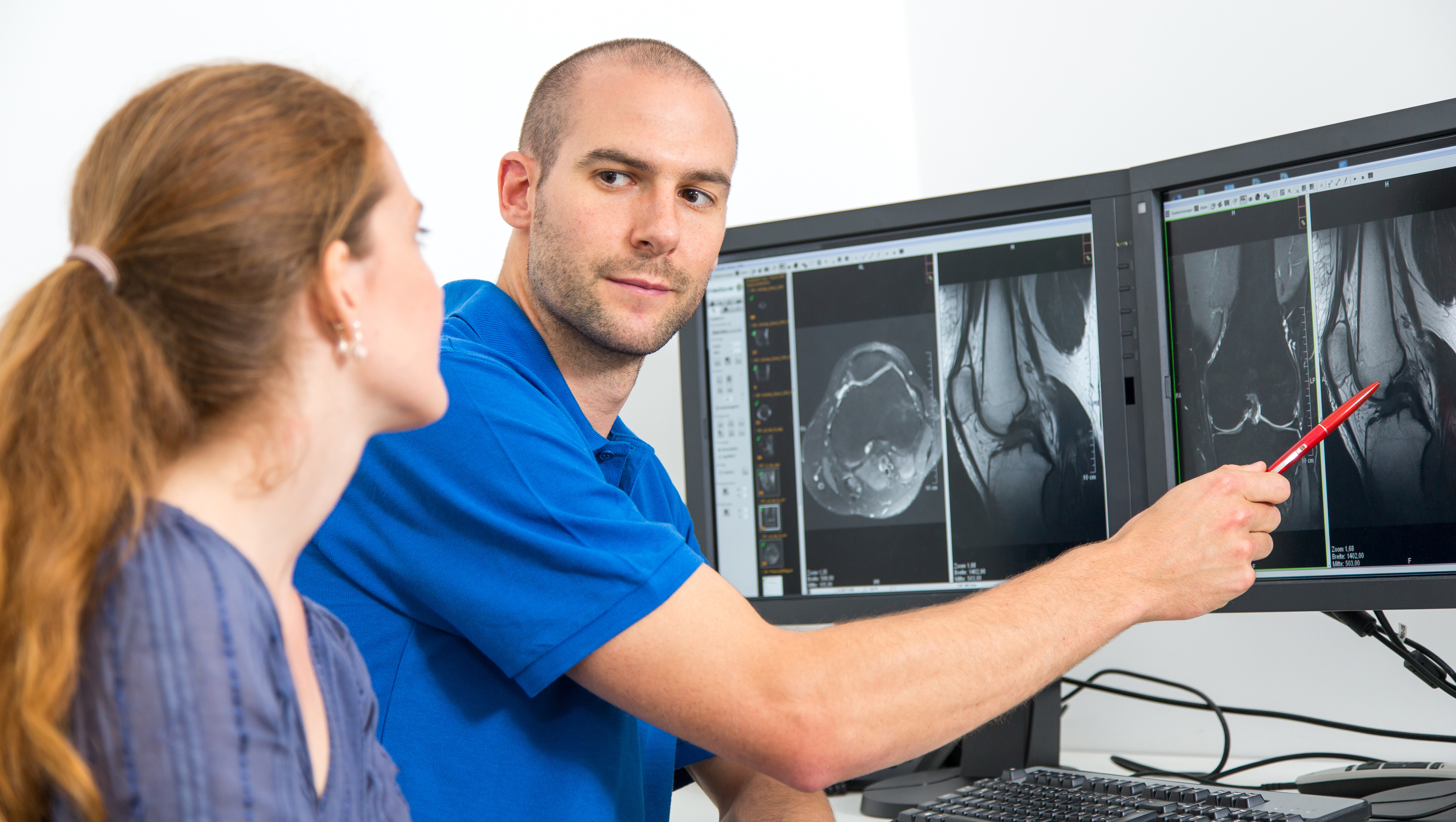
The radiology community is abuzz with talk of artificial intelligence (AI) systems that can assist physicians with image interpretation and perform other tasks. Like any new technology, it will take time before AI gains widespread acceptance due to the cost of implementation. This is analogous to the early-day PACS, where the benefits of efficiency had to be proven in order to justify the expenditure for such a costly system. Today almost all imaging is interpreted on computer systems … when was the last time anyone looked at a piece of film?
Reimbursement for Artificial Intelligence in Radiology is More Than Just Billable Codes on April 5, 2021
Categories: radiology reimbursement, radiology, AI
Update on The Quality Payment Program on March 17, 2021
The Quality Payment Program (QPP) continues to be modified due to the COVID-19 public health emergency. The Centers for Medicare and Medicaid Services (CMS) recently announced some leeway for clinicians affected by the pandemic in 2020 and 2021.
Categories: radiology reimbursement, cms, QPP, COVID-19
The issue of patients receiving large, unexpected medical bills from hospitals and physicians has been widely publicized. This situation, known as surprise billing, arises when a hospital or physician provides medical care to a patient but is not participating in a patient’s insurance network. We have reported on the many states that have put legislation in place to try and mitigate the problem for their own residents, but now there will be a nationwide policy thanks to recent federal legislation.
Categories: radiology reimbursement, radiology, surprise billing
Understanding the Impact of The Medicare Fee Schedule for 2021 on Your Radiology Practice on January 25, 2021
When the Medicare Physician Fee Schedule (MPFS) Final Rule was published in December, it looked like radiology was facing a significant cut in Medicare reimbursement for 2021. Our article reported that professional component fees would drop 10-11% while global reimbursement would see a lesser impact. The Consolidated Appropriations Act, 2021 (CAA) rolled back those cuts at least for 2021, although the Medicare fee schedule for radiology will likely continue to be adjusted downward in the future as implementation of the revalued Evaluation and Management (E&M) services is fully phased in.
Categories: radiology reimbursement, medicare, medicare reimbursement, MPFS, radiology
How the Consolidated Appropriations Act Will Impact Radiology Practices on January 18, 2021
The “Consolidated Appropriations Act, 2021” (CAA) is a sweeping piece of legislation that provides relief to individuals and businesses impacted by the COVID-19 public health emergency. Some of the relief provisions apply to all businesses, including medical practices, but it also contains several measures that specifically apply to medical practices.
Categories: radiology reimbursement, medicare, medicare reimbursement, radiology, surprise billing, Paycheck Protection Program
Major Cut in Radiology Reimbursement For 2021 Is Finalized By CMS on December 7, 2020
The Centers for Medicare and Medicaid Services (CMS) has released the final set of rules that will govern the Medicare payment system for the coming year, thereby affirming the drastic cut in radiology reimbursement for 2021 that was proposed earlier this year. There were few surprises in the Medicare Physician Fee Schedule (MPFS) Final Rule that were not contained in the proposed rule, other than a slight improvement in the fee schedule conversion factor and a change to the QPP Performance Threshold.
Categories: radiology reimbursement, cms, MPFS, radiology, QPP
ICD-10 Coding Changes For 2021 That Will Impact Radiologists on November 13, 2020
There are 490 new ICD-10-CM[i] codes that became effective on October 1, 2020, all of which are replacing existing codes. An additional 47 codes have been revised and 58 were deleted. Two new codes, U07.1 for COVID-19 and U07.0 for vaping-related disorders, took effect on April 1, 2020. They are contained in a new section of the guidelines, Chapter 22 “Codes for Special Purposes (U00 – U85)”.
Categories: radiology reimbursement, icd-10, radiology
Can Radiologists Effectively Bill for COVID-Related Costs? on October 14, 2020
Radiologists practicing in an imaging center or other non-hospital facility have a new tool available that will potentially allow them to recover some of the added costs related to safety precautions taken during the COVID-19 public health emergency. CPT code 99072 was added by the American Medical Association (AMA) Current Procedural Terminology (CPT®) Editorial Panel on September 8, 2020, with immediate effect. While payment for this code is not yet available from Medicare, it might be reimbursed by some commercial payers.
Categories: radiology reimbursement, radiology, COVID-19
Get Feedback on Your 2019 Quality Payment Program Performance on September 22, 2020
Quality Payment Program (QPP) participants can now obtain information about whether their practice will receive a positive, negative, or neutral Medicare fee schedule adjustment in 2021 based on the 2019 data they submitted. The Centers for Medicare and Medicaid Services (CMS) announced that clinicians who participated in the Merit-based Incentive Payment System (MIPS) in 2019 can access their performance feedback by logging in to the Quality Payment Program website.
Categories: radiology reimbursement, physician reimbursement, cms, Quality Payment Program, QPP, quality measures
Radiology’s Declining Reimbursement Spans More Than A Decade on August 20, 2020
The average cut of 11% in radiology reimbursement that is proposed by the Medicare Physician Fee Schedule for 2021 (MPFS) is the continuation of a trend that spans more than a decade.
Categories: radiology reimbursement, medicare, medicare reimbursement, MPFS, radiology