By now everyone involved in billing Medicare for physician services should be aware of the new Quality Payment Program (QPP) that will be in effect for payments in 2019 based on data submitted in 2017. The proposed rules for the new system were outlined in our recent article Medicare Quality Reporting Rules are Changing. The final regulations that will govern the new system were recently issued, and radiology practices will benefit from preparing as early as possible to capture the data they will need to report under the new system.
Most radiology practices will report their data under the Merit-based Incentive Payment System (MIPS), and this series of articles outlines the steps you need to follow in order to maximize your 2019 Medicare reimbursement. Practices that are members of an Accountable Care Organization (ACO) might have the option to report as an advanced Alternative Payment Model (APM) through that system, however the regulations indicate that many of the current ACOs will not qualify or only partially qualify and so MIPS appears to be the most practical of the two alternatives for most physicians.
Under MIPS there are four performance categories: Quality, Advancing Care Information (ACI), Clinical Practice Improvement Activities (IA), and Cost. Of these, the largest component is Quality. For 2017 the Quality Performance Category is worth 60% of the total points needed to maximize your score under MIPS because the Cost Category will not be in effect for the initial year of MIPS and its 10% value has been reallocated to Quality. For 2018, Quality is expected to be returned to 50% of the total score and then reduced to 30% in 2019. This article will outline the basics of the Quality Performance category.
Selecting the Measures
Eligible Clinicians (ECs) are required to choose six quality measures to report, although more than six may be submitted for consideration in order to determine the six that have the highest quality scores. One of the measures must be an outcome measure, or another high quality measure if no outcome measure is available. For radiologists, most outcome measures are not likely to apply so you must choose at least one measure that is categorized as high priority. No crosscutting measures are necessary, as this requirement has been removed for MIPS in 2017.
The quality measures are selected by the EC or group practice from the standard set of individual measures or from a specialty measure set, all of which are the same as those available for 2016 reporting under PQRS. There are 32 measures that are potentially applicable to radiology. Of these, 13 are available through claims submission and 19 are available only through registry submission. Some may be listed under either ‘surgical’ or ‘cardiology’ measures sets. The measures are available from CMS in Table E of the MACRA Final Rule.
In order to maximize scoring, it would be best to choose measures that have benchmarks. This will allow up to 10 points to be earned for each measure, otherwise only 3 points will be possible for the measures without benchmarks.
Reporting measures under the Quality Performance category of MIPS is essentially the same as it was under the Physician Quality Reporting System (PQRS) it is replacing. Under PQRS, 9 measures from across 3 domains were required, whereas only 6 measures with no domain restrictions are required under the new program. However, under PQRS the result was “all or nothing”, meaning that all of the required measures had to be reported successfully in order to avoid a payment penalty. Under MIPS, each measure will be graded individually to contribute to the total score. If 6 measures are available to be reported and less than 6 are actually reported, any unreported measures will add zero points to the score.
Reporting the Measures
Eligible Clinicians may submit their quality measures data either individually or as part of a group practice, no later than March 31, 2018 for the 2017 reporting period. Submitting via regular Medicare claims is available only to ECs reporting as individuals. If the claims method is selected, 50% of the EC’s Medicare patients would have to be reported. For all other reporting methods, 50% of patients from all payers must be reported. The reporting methods that will be available for 2017 are as follows:
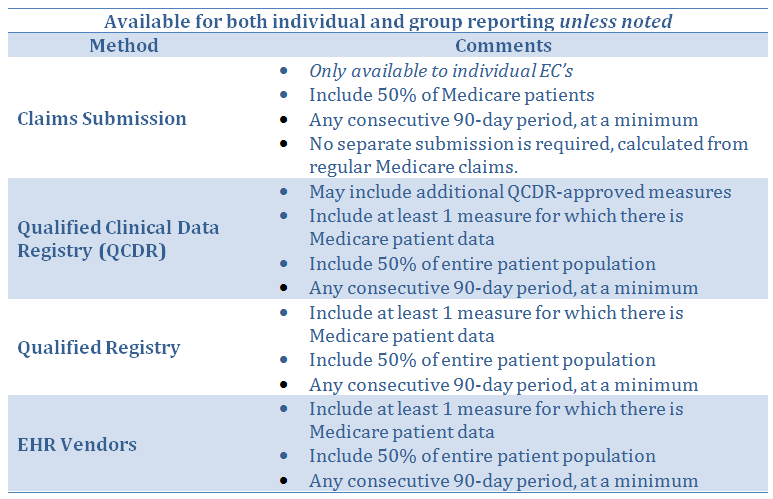
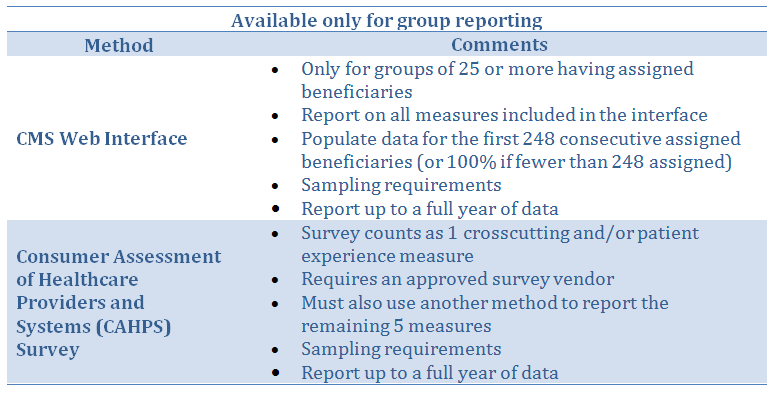
One population measure, which pertains to All Cause Hospital Readmissions, is applicable only to groups of 15 or more ECs, and there is no action required on the part of the group. “Administrative Claims” will be used by CMS to automatically determine if the population measure applies to the practice, and CMS will automatically calculate it. Since it is based on primary care services it will not apply to radiologists.
Scoring the Quality Measures Reported
Each measure is worth up to 10 points, so the 6 highest quality measures reported plus the population measure as determined independently by Medicare (if applicable) combine to determine the number of available points from up to 60 or 70 points.
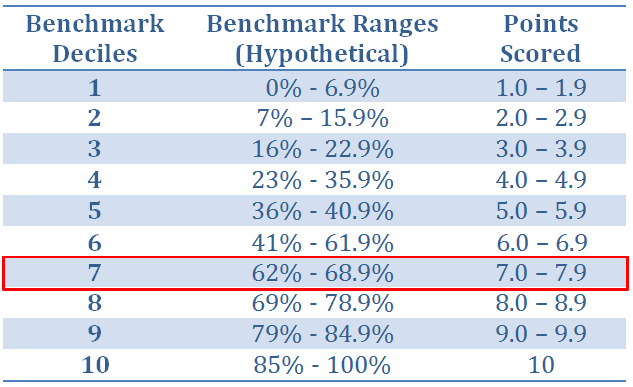
Points will be earned based on the EC’s percentile-basis performance on each measure compared with national peer benchmarks. The following is a breakdown of the scoring for each measure:
- Starting from an overall average benchmark percentage and working forward to 100% and backward to 0%, each measure is broken down into percentage ranges and assigned to deciles from 1 to 10 (see the example table below).
- The higher the performance score percentage on a measure, the higher the decile to be awarded.
- Each decile is scored in a range from x.0 to x.9 based on where a measure’s performance falls within the benchmark range. For example, using the table below, a measure performance rate of 38.5% will fall within decile 5 so the measure will be awarded between 5.0 and 5.9 points out of the possible 10 points.
The points earned for all measures are summed up. A measure that is not reported will generate zero points, thus lowering the total score but not eliminating the EC from passing the Quality category entirely.
In addition to points earned based on performance on the 6 quality measures reported, up to 6 Bonus Points are available based on the measures types and up to 6 additional bonus points will be available for end to end electronic reporting. Note that the bonus for end to end electronic reporting will most likely not be available to radiologists since their quality data is usually obtained through dictated reports and not initiated from the electronic health record.
- Two bonus points will be awarded for reporting each ‘outcome’ measure beyond the one required.
- Two bonus points will be awarded for reporting each patient experience measure.
- One bonus point will be awarded for each ‘high priority’ measure reported, limited to 10% of the total available points.
- One bonus point will be awarded for each measure that is reported demonstrating ‘end to end electronic reporting’ using Certified Electronic Health Record Technology (CEHRT), limited to 10% of the total available points.
Bonus points can be obtained for reporting high priority measures in addition to the points earned for using those same measures in the 6 highest scoring measures. Bonus points are only awarded for measures reported that meet the reporting completeness requirements during the reporting period: 50% of claims are reported, the performance rate is not 0%, and a minimum of 20 cases are reported.
The points earned through reporting measures plus any available bonus points are combined, and divided by the total possible points to obtain the overall Quality Performance Score for the Quality category. For example, a doctor earned 41.9 points based on the 6 quality measures, 6.3 points assigned through the patient population measure, 1 bonus point for choosing a high-priority measure and 3 bonus points for reporting 3 measures using end to end electronic reporting using a CEHRT, for a total of 52.2 points. Dividing this total by the 70 possible points (10 for each of the 6 quality measures and 10 for the one population measure the doctor qualified for) gives a Quality Performance score of 74.6%.
Contribution to the Final Score
The Quality Performance category is worth 60% of the EC or group’s overall Final Score under MIPS for 2017. Continuing with the example above, the EC earned a 74.6% quality performance score which, when multiplied by the 60 points for this category, earns the physician 44.8 points toward the total of 100 maximum points under MIPS.
In addition to Quality Performance, the Advancing Care Information (ACI) category is worth 25% and the Clinical Practice Improvement Activities (IA) category is worth 15%. The Quality Performance component could become even more important if a radiologist can claim an exclusion from the ACI category (formerly EHR Meaningful Use), in which case the 25% allotted to that category could be redistributed to the Quality category as well. (Refer to our article in this series on ACI for more information.) Thus, Quality Performance could potentially become 85% of the total and the doctor in our example would earn 63.4 points (74.6% multiplied by 85 points) toward the 100 needed to maximize the MIPS score. The Cost category has been re-weighted to zero for 2017.
How to Prepare for Quality Performance Reporting
Since this category alone could be the major determinant of a radiology EC’s reimbursement adjustment under MIPS, it’s not too early to begin to define the systems and processes that will be needed to gather the data for measures reporting. Practices that have been reporting under PQRS are ideally suited to be able to comply with the new rules under MIPS.
First, it would be a good idea to review the available measures and determine which ones will allow the individual ECs or the group to achieve their best performance score.
Next, review the reporting options and determine which method will be best suited to your practice. Radiologists might consider group reporting to ensure selection of the best 6 measures across the group to meet 20 case thresholds required to score a measure (otherwise the measure score will default to 3 points) and thereby maximize scoring.
Special Transitional Rules for 2017
This article describes the criteria and steps a practice can use to maximize its score and obtain the highest upward fee schedule adjustment from Medicare for 2019. For those ECs who cannot fully comply with all of these requirements, or who simply choose to defer full compliance until 2018, CMS has announced the minimum requirements necessary in order to avoid a 4% payment penalty in 2019. Known as the Pick Your Pace transitional rules for 2017, the options are as follows:
- Test the QPP by submitting one measure from the Quality, IA or the base measures from the ACI categories. An EC does not need to meet data completeness standards such as the 50% threshold or the minimum 20-case threshold in order to avoid the penalty.
- Submit more than one measure for a portion of the 2017 calendar year (for a minimum of a continuous 90-day period) and potentially earn a small positive payment adjustment. This will allow ECs who might not be ready at the beginning of the year to ramp up to full participation later in the year and be fully ready for 2018.
- Full participation in MIPS for at least a 90-day period during 2017, such as we have described in this article for the Quality component as well as any additional MIPS categories that apply (ACI, IA), will qualify ECs and groups for the highest positive payment adjustment in 2019.
Maria Calamaro serves as Product Director for Healthcare Administrative Partners and is the company’s subject matter expert for CMS quality programs. She has over 20 years of experience leading the product development and direction-setting for physician and hospital healthcare applications.
Subscribe to this blog to stay current with developments in the new MIPS program. Our next installment in this blog series will review the requirements of the Clinical Practice Improvement Activities (IA) component of MIPS.
Related articles:
Medicare Quality Reporting Rules are Changing
Transitioning Your Radiology Practice to MIPS: Advancing Care Information