 Healthcare Administrative Partners continues our efforts to help radiology practices make a successful transition to ICD-10 with this article, the third in our series focusing on how radiologists can fine-tune their documentation to assure the best coding and uninterrupted reimbursement. Our previous articles covered Documentation for Pain and Documentation for Fractures and our blog contains additional information to help radiology practices prepare for this major change.
Healthcare Administrative Partners continues our efforts to help radiology practices make a successful transition to ICD-10 with this article, the third in our series focusing on how radiologists can fine-tune their documentation to assure the best coding and uninterrupted reimbursement. Our previous articles covered Documentation for Pain and Documentation for Fractures and our blog contains additional information to help radiology practices prepare for this major change.
Documentation Requirements for Neoplasms
Although the coding of neoplasms in ICD-10 is not dramatically different from the coding in ICD-9, radiologists must be aware of certain aspects of documentation that will assist the coding team in identifying the most specific diagnosis code possible as the new standard mandates.
Here are some documentation reminders that will allow for proper coding of Neoplasms under ICD-10:
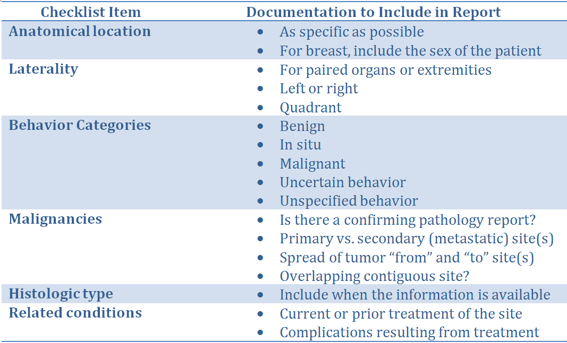
A thorough patient history pertinent to the exam is more important for ICD-10 coding than ever before, and especially for radiologic exams of neoplastic tumors. The general areas that must be covered when documenting such exams include the specific anatomical location (with laterality for paired organs), behavior categories, and metastatic sites when applicable. Coders will also need to know whether the imaging is of the primary or a secondary site, if the patient is undergoing treatment for the current condition, or if treatment was completed previously.
Exams to evaluate breast neoplasms require the sex of the patient for proper coding. While this information is usually present in the demographics, it makes the coder’s job easier and more efficient if it is also included in the body of the report.
In order to use the ICD-10 codes indicating a malignancy the medical record must contain a pathology report with a confirmed malignancy diagnosis, and the radiologist should dictate into the report whether or not such a report exists. When a radiology report indicates the diagnosis of mass, growth, tumor or neoplasm alone, the coder will be forced to apply a code of “unspecified”. The use of an unspecified code is not acceptable if there is one that can be more specific, so the more information that can be included in the radiology report, the better the coding will be. This will assure appropriate reimbursement.
Practice Workflow Considerations
The information coming from ordering physicians will likely improve as they become more knowledgeable about the requirements of ICD-10, and they might even be able to provide the coding used in their own charts. Reception and scheduling staff should be trained to ask for more specific information about the patient’s history and reason for the referral. In the case of tumor diagnosis, specific coding will not necessarily be available for the initial imaging ordered but by the time higher-end exams such as MRI, CT and PET/CT are being ordered there will be more diagnostic information available, perhaps including ICD-10 codes.
Technologists are in the best place to obtain history and information about related conditions and treatments directly from the patient at the time of the exam. Tech worksheets can be constructed to include prompts for these details, and then radiologists must dictate the relevant information into the report.
Conclusion
The biggest change in the documentation of exams for evaluation of neoplasms is the need to be as specific as possible about the site of the tumor, the laterality and/or quadrant when appropriate, and whether the site is primary or secondary. If a pathology report confirms a malignancy, then this fact should be in the radiology report. Any other details about the nature of the tumor or its treatment will help coders apply the most specific ICD-10 code possible. This kind of documentation will maximize reimbursement from any and all payers.
Our series on ICD-10 documentation for radiology practices will conclude with an article containing coding tips and considerations for a variety of exam types, as well as a summary of the key recommendations from the topics already covered. Be sure to subscribe to this blog so you won’t miss any information that will help you maximize reimbursement under ICD-10.
Related articles:
Preparing Your Radiology Practice for the ICD-10 Transition - How to Document Pain
Preparing Your Radiology Practice for the ICD-10 Transition - Documentation for Fractures




