Reimbursement rates for both Breast Ultrasound and Digital Breast Tomosynthesis (DBT) received a boost from the Centers for Medicare and Medicaid Services (CMS) this year. Medicare adopted new CPT1 coding that provides enhanced reimbursement for ultrasound services, and coverage was newly approved for DBT as an add-on to screening and diagnostic mammography examinations. These changes were described in our article, The Impact of Coding Changes on Radiology Practices in 2015. In order to fully realize the benefit of these new billing opportunities, proper documentation is required within radiology practices.
from the Centers for Medicare and Medicaid Services (CMS) this year. Medicare adopted new CPT1 coding that provides enhanced reimbursement for ultrasound services, and coverage was newly approved for DBT as an add-on to screening and diagnostic mammography examinations. These changes were described in our article, The Impact of Coding Changes on Radiology Practices in 2015. In order to fully realize the benefit of these new billing opportunities, proper documentation is required within radiology practices.
Breast Ultrasound
The new ultrasound coding delineates a complete exam (76641) from a limited exam (76642), replacing the previous non-specific code (76645) that provided one level of reimbursement for any type of breast ultrasound study. An imaging center will gain 21.4% when billing globally for a complete vs. a limited breast ultrasound examination (using the national Medicare fee schedule in effect for January – June, 2015). Most of the benefit comes from the technical component, but radiologists in a hospital setting will gain 7.1% in their professional component by including complete documentation in their reports.
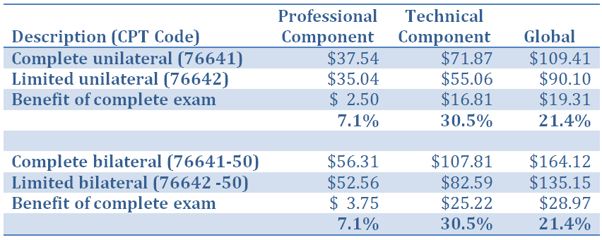
Note that the new codes are for unilateral examinations. When medical necessity determines that a bilateral study is indicated, Medicare will increase reimbursement to 150% of the unilateral rate when a modifier (-50) is added to either code. Other payers (notably Medicaid) do not accept the -50 modifier and will require separate claim lines billed with the LT and RT modifiers to indicate the left and right breast.
Regardless of the coding used, full and complete imaging and documentation must be included for each breast separately. According to the American College of Radiology, a complete examination must include all four quadrants of the breast and the retroareolar region. It also includes ultrasound examination of the axilla, if performed. A study that does not meet these criteria is considered to be limited.
The complete code will be denied unless all of the criteria are met. This will result in no reimbursement at all until the claim is re-billed with the limited code; however, this would result in reimbursement lower than expected and also a delay in payment due to the reprocessing. The best solution is to provide complete documentation in the first place.
The new ultrasound coding structure is available for all payers, not only Medicare. Be aware, though, that some payers will delay adoption of the new codes, instead continuing to recognize only the obsolete 76645 -- and reimbursement will be delayed if the new codes are used.
While radiologists are pleased with the new, higher reimbursement levels associated with these codes, patients are not as happy because they have higher co-insurance that is based on a percentage of the new allowed charges. For payers that require separate claims for bilateral ultrasound, patients will see two co-payments or co-insurance amounts instead of the single charge they had seen in the past. Practices should be prepared to answer questions about increased out-of-pocket costs from their patients who have had previous breast ultrasound exams.
Digital Breast Tomosynthesis (DBT)
Sometimes referred to as 3-D Mammography, DBT is cutting-edge technology that is not yet available at every imaging center or hospital since insurance reimbursement for it has been largely unavailable. Medicare’s reimbursement of DBT beginning in 2015 is $30.39 for the professional component and $56.13 when billed globally (using the national Medicare fee schedule in effect for January – June, 2015) for code 77063 (screening) or G0279 (diagnostic). These payments are made in addition to the regular reimbursement for the associated digital mammogram.
Documentation of DBT must be included in conjunction with either a screening or diagnostic digital mammogram for reimbursement under the new Medicare rules, since the codes that CMS has defined are to be used as add-on codes. There is no way to receive reimbursement from Medicare for a stand-alone DBT exam when it is performed separately. If and when other payers adopt payment policies for DBT they will have the option to use the CPT codes differently, which will certainly create confusion among radiology coding and billing professionals.
Claims for DBT reimbursement may only be submitted if the documentation of the exam is adequate. The following examples of mammography reports include the recommended documentation for DBT that will satisfy the requirements for full reimbursement.
Diagnostic Mammogram Report, including DBT:
Screening Mammogram Report, including DBT:
Both of these examples include documentation of the use of computer-aided detection (CAD) in the review of the images. This is another add-on charge using code 77052 that will generate $3.22 in professional component and $8.94 globally from Medicare in addition to the basic digital mammogram and DBT charges, but only when its use is documented in the report.
Medicare’s coverage of DBT may begin to turn the tide with other payers, but as of now most of the major payers still consider this to be “unproven and not medically necessary”, in the words of United Healthcare’s Medical Policy Manual. This is reminiscent of the advent of digital mammography, where the cost of entry into the technology was very high but those who adopted it early received the benefit of higher reimbursement from Medicare that helped cover that entry cost. Once Medicare began its coverage of digital mammography, other payers followed suit quickly.
When a payer denies coverage for DBT, the practice’s ability to bill patients for the services will depend upon the individual payer’s policy. Most of the major payers that deny are doing so as a contractual adjustment, which means that practices must write-off the charge. A few, such as Highmark Blue Shield of PA and United Healthcare, are denying DBT as experimental but indicate that the patient is responsible for payment. It is always beneficial to notify patients in advance if they may experience more out-of-pocket expense than their normal co-payment or co-insurance. The coverage situation will change over time, so careful attention to payer policies and analysis of denials is required. Be sure to subscribe to this blog for the latest news on such policy changes.
Without the proper documentation, radiologists will lose this added revenue from Medicare for breast ultrasound and digital breast tomosynthesis services. Radiology practices should ensure that their staff and outsourced billing vendors are current on these issues in order to maximize reimbursements today and into the future.
1 Current Procedural Terminology (CPT) is a copyrighted code set developed and maintained by the American Medical Association.




