 As with any medical procedure, the performance of abdominal ultrasound examinations is defined by specific practice parameters. Likewise, the documentation of those exams must also comply with certain criteria in order for the practice to realize full reimbursement for them. The accepted guideline1 for the performance of abdominal or retroperitoneal ultrasound exams indicates, “Depending on clinical indications, an examination may include the entirety of the abdomen and/or retroperitoneum, a single organ, or several organs.” Similarly, the documentation must contain an exact description of the procedure for proper billing.
As with any medical procedure, the performance of abdominal ultrasound examinations is defined by specific practice parameters. Likewise, the documentation of those exams must also comply with certain criteria in order for the practice to realize full reimbursement for them. The accepted guideline1 for the performance of abdominal or retroperitoneal ultrasound exams indicates, “Depending on clinical indications, an examination may include the entirety of the abdomen and/or retroperitoneum, a single organ, or several organs.” Similarly, the documentation must contain an exact description of the procedure for proper billing.
A study2 conducted by Richard Duszak, Jr., M.D. and his colleagues reviewed over 100,000 abdominal ultrasound exams and found that only 87.4% of those billed as “complete” contained sufficient documentation to support a complete exam. Incomplete documentation will have a negative financial impact on the practice, either because the initial billing will be at a lower (limited) level or following an audit that finds the deficiencies, penalties will be incurred on top of fee refunds that may sometimes span many years of billing.
Failure to perform or document a complete abdominal ultrasound exam will result in lower reimbursement as a “limited” study rather than a “complete” study. The following table gives an example of the financial benefit of including the proper documentation in order to receive the correct reimbursement (or, conversely, the financial loss for not properly documenting):
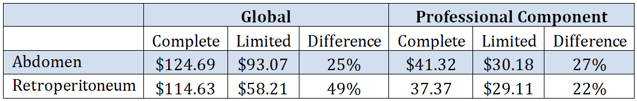
This table uses the Medicare national payment level as of July 2015.
When the radiologist fails to adequately document a complete abdominal ultrasound, he or she will lose 27% of the professional component reimbursement. In the imaging center, the loss for incomplete documentation of a retroperitoneal ultrasound would be 49% of the reimbursement. It pays to know the rules of documentation and follow them.
Note that medical necessity will always be the governing factor in the performance, and therefore in the documentation, of the exam. When the order is for a specific organ or organs, then the exam will include only the requested elements and it will be properly billed as a limited exam of those requested areas. It is always important for the final billing to match the exams that are ordered.
A complete ultrasound examination of the abdomen includes imaging and documentation of all of the following:
- Liver
- Gall bladder
- Common bile duct
- Pancreas
- Spleen
- Kidneys
- Upper abdominal aorta
- Inferior vena cava
The documentation must also include any demonstrated abdominal abnormality. If one of the listed elements cannot be imaged, for example due to its surgical removal or because it is obscured, then the exam will still be considered to be complete if the report includes a description of the reason it is missing.
A complete ultrasound examination of the retroperitoneum includes imaging and documentation of all of the following:
- Kidneys
- Abdominal aorta
- Common iliac artery origins
- Inferior vena cava
Note that if the clinical history suggests urinary tract pathology, then a complete evaluation of the kidneys and urinary bladder also comprises a complete retroperitoneal ultrasound. In either case, including less than the required elements in the documentation for a “complete” exam will cause it to be billed as a “limited” exam. Dr. Duszak’s study recommends structured reporting as one way a radiology practice can avoid missing essential documentation elements.
Abdominal imaging might also include Doppler evaluation of blood flow characteristics, which might be separately billable provided there is medical necessity and adequate documentation. Our article Duplex Doppler Ultrasound Tips to Help Maximize Radiology Reimbursements contains information to help the radiologist include all of the required documentation elements.
In summary, when a complete ultrasound exam is ordered and performed, there are certain minimum requirements that must be met. The documentation of the exam has to include a description of all of the elements, or the result will be lower revenue since it will be billed as a limited exam. Duplex Doppler imaging, when performed, has to be thoroughly documented along with the underlying abdominal exam. Structured, standardized reporting is one technique radiologists can adopt to help assure that all of the required reporting elements are included. Practices can develop templates to be sure that the guidelines are followed for each and every case. With repetition of good documentation habits, full and complete documentation will become second nature.
1 The Practice Guideline for the Performance of an Ultrasound Examination of the Abdomen and/or Retroperitoneum, published in 2012, was developed jointly by the American College of Radiology (ACR), the American Institute of Ultrasound in Medicine (AIUM), the Society for Pediatric Radiology (SPR) and the Society of Radiologists in Ultrasound (SRU).
2 Physician Documentation Deficiencies in Abdominal Ultrasound Reports: Frequency, Characteristics, and Financial Impact, Journal of the American College of Radiology, June 2012.
Related articles:
Learn the Proper Documentation for 3D Reconstruction to Maximize Radiology Practice Reimbursement
Documentation Diligence is the Key to Radiology Practice Reimbursement




