 This is the third in our series of articles designed to help radiology practices prepare for the Merit-Based Incentive Payment System (MIPS). Previous articles covered the Quality Performance Category, which is the largest portion of the MIPS score, and the Advancing Care Information (ACI) Category. Quality will initially account for at least 60% of the total MIPS score and ACI will account for up to 25% of the total score. The Improvement Activities (IA) Category, originally called the Clinical Practice Improvement Activities in proposed regulations, represents 15% of the total score for 2017, the first year of MIPS participation. The fourth element of MIPS, the Cost Category, has been reweighted to zero for 2017.
This is the third in our series of articles designed to help radiology practices prepare for the Merit-Based Incentive Payment System (MIPS). Previous articles covered the Quality Performance Category, which is the largest portion of the MIPS score, and the Advancing Care Information (ACI) Category. Quality will initially account for at least 60% of the total MIPS score and ACI will account for up to 25% of the total score. The Improvement Activities (IA) Category, originally called the Clinical Practice Improvement Activities in proposed regulations, represents 15% of the total score for 2017, the first year of MIPS participation. The fourth element of MIPS, the Cost Category, has been reweighted to zero for 2017.
As most Eligible Clinicians (EC) already know, MIPS will begin to take effect for Medicare physician reimbursement in 2019 but those payment adjustments will be determined by performance reported for 2017, which is being termed a ‘transitional year’ for the program. The reporting period for 2017 has been lowered to a minimum of 90 days rather than a full year for all of the MIPS categories. It is expected that MIPS will be in full effect for 2018.
Overview of the Improvement Activities (IA) Category
According to the Centers for Medicare and Medicaid Services (CMS) Final Rule governing the MIPS, Improvement Activities are “those that support broad aims within healthcare delivery, including care coordination, beneficiary engagement, population management, and health equity.” These activities have been identified as improving clinical practice or care delivery, and are likely to result in improved health outcomes. There are 92 such activities available from which EC’s may choose for 2017, each with a weight of either “High” or “Medium”.
High-weighted activities are worth 20 points each, and medium-weighted activities are worth 10 points each. To earn full credit for the IA category, a total of at least 40 points from any combination of activities is required – for example, 4 medium-weighted, 2 high-weighted, or 2 medium- and 1 high-weighted.
For certain practices and EC’s, the value of each activity is doubled so that high-weighted activities are worth 40 points and medium-weighted activities are worth 20 points. Thus, only 1 high-weighted activity or 2 medium-weighted activities would be necessary. These practices and EC’s include:
- Small practices of fewer than 15 EC’s
- EC’s located in a rural or health professional shortage area
- EC’s who are “non-patient facing”
An EC will be considered “non-patient-facing” (NPF) if he or she has 100 or fewer Medicare Part B patient-facing encounters during the annual determination period. The initial determination period is September 2015 to August 2016 for the 2017 reporting period, with a second determination period of September 2016 to August 2017 to identify additional ECs who qualify as NPF. Medicare will automatically determine whether an EC is classified as patient-facing or non-patient facing based on CPT codes submitted; no action on the part of the EC is required. Once an EC has been classified as NPF for a reporting period, he or she will continue to be considered NPF for the remainder of that reporting period. In other words, the second determination period cannot cause the removal of the NPF classification.
The majority of radiology practices will be considered NPF and therefore will have to complete fewer Improvement Activities under MIPS. We discussed this topic more thoroughly in our recent article, Why the MIPS Patient-Facing Rules are Important to Radiologists.
Choosing Improvement Activities
The IA list includes 14 high-weighted and 78 medium-weighted activities within these 8 sub-categories:
- Achieving Health Equity (4 activities)
- Behavioral and Mental Health (8 activities)
- Beneficiary Engagement (23 activities)
- Care Coordination (14 activities)
- Emergency Response and Preparedness (2 activities)
- Expanded Practice Access (4 activities)
- Patient Safety and Practice Assessment (21 activities)
- Population Management (16 activities)
The choice of activities will depend on each practice’s structure and data-gathering capabilities. Radiology practices will only have a small subset of the 92 possible improvement activities that directly relate to their clinical practice, with the most applicable falling in the Beneficiary Engagement, Care Coordination and Patient Safety and Practice Assessment (and possibly the Expanded Practice Access) sub-categories. The other sub-categories contain few activities that will apply to radiology in 2017.
Within the applicable sub-categories, radiologists will find about a dozen that may be relevant, yet fewer that are actually achievable in the short run. Many activities will require the use of a Qualified Clinical Data Registry (QCDR) for reporting, along with new technology and changes to workflow processes to gather the requisite data. The good news is that in the early years of MIPS very few activities will be needed to satisfy the IA category, especially when using group reporting. Over the longer horizon, radiology practices should put a plan in place to address those activities that are of interest but not currently feasible so that they can be attained in subsequent years of MIPS.
We have identified the following as a few of the activities that radiology practices may want to consider being applicable:
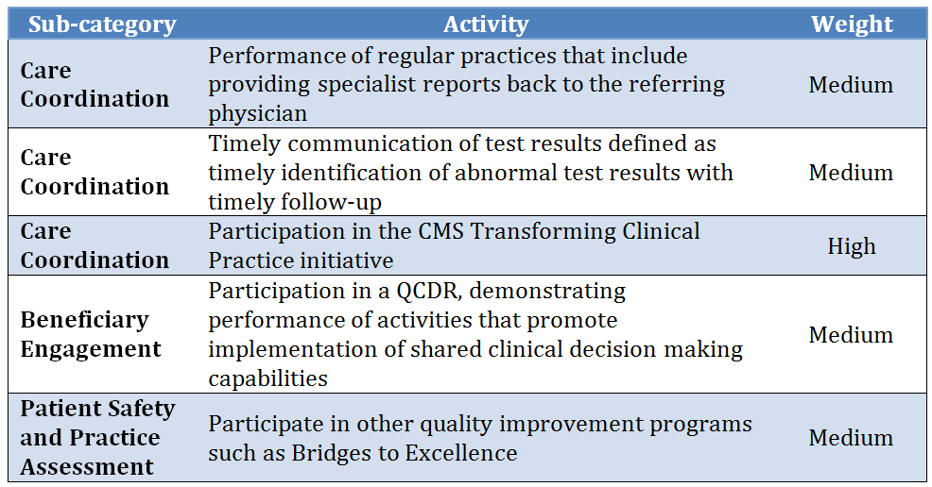
The full listing of Improvement Activities available for 2017 is contained in Table H of the CMS Final Rule, and it is reproduced here on the CMS Quality Payment Program web site.
CMS has not yet provided any specifics about how each of the activities should be performed in practice to successfully satisfy the requirements. It is therefore up to the individual EC or practice to determine the method of implementation, tracking and documentation to substantiate its performance for potential audit purposes. More guidance will become available through specialty societies and from CMS as time goes on.
Reporting Improvement Activities
The decision to report as individual ECs or as a group will require some balancing of pros and cons, and it will require a comprehensive look at all of the MIPS categories since reporting must be done consistently using one method or the other across all of the categories. For the IA category, when reporting as a group only one EC in the group needs to perform each selected activity and the entire group receives credit! This provides a heavy advantage to group reporting over individual EC reporting in the IA category, especially for larger groups.
The reporting of Improvement Activities will be done following the end of the year by attesting that the activities were completed through the use of a CMS-provided attestation system. This method is very similar to the previous CMS programs such as Meaningful Use, and it requires that documentation be kept to prove that activities were performed in the event of an audit by CMS.
Conclusion
Unlike Quality Performance and Advancing Care Information, which replace older CMS programs, the Improvement Activities category is totally new and it will take some time to be fully understood. The following are some key concepts for radiology practices to remember about the IA category:
- Radiology practices with fewer than 15 ECs and those who are considered non-patient facing only need to report 1 high-weighted or 2 medium-weighted IAs to receive the full credit of 40 points.
- Only about a dozen or so improvement activities are currently applicable to radiology, and few are high-weighted.
- Most applicable IAs will be found in the Beneficiary Engagement, Care Coordination and Patient Safety and Practice Assessment categories.
- Group reporting provides an advantage since a single individual’s participation gives credit to the entire group.
Gathering the data for some IAs is labor-intensive and may require QCDR reporting, additional technology, and enhanced workflows – which may be a stretch for practices in the near term. Practices should select the activities most readily achievable today and put a plan in place for future compliance with additional activities most meaningful to their clinical practice goals.
Although the performance year of 2017 allows for less than full participation, a higher level will be required in the years that follow. Our goal at HAP is to help radiologists maximize reimbursement by fully complying with all MIPS performance categories, and by doing so as early as possible you will be in the best position to achieve optimized reimbursement in the future.
Maria Calamaro serves as Product Director for Healthcare Administrative Partners and is the company’s subject matter expert for CMS quality programs. She has over 20 years of experience leading the product development and direction-setting for physician and hospital healthcare applications.
Related articles:
Transitioning Your Radiology Practice to MIPS: The Quality Component Updated
Transitioning Your Radiology Practice to MIPS: Advancing Care Information



