 The Merit-Based Incentive Payment System (MIPS) is slowly being analyzed and absorbed by the medical community. This system, passed into law by the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), will begin to take effect for physician reimbursement in 2019 but those payment adjustments will be determined by performance in various categories for services rendered in 2017. Regulations governing the application of this law have now been finalized and savvy radiology practices can begin to prepare to comply with the new system.
The Merit-Based Incentive Payment System (MIPS) is slowly being analyzed and absorbed by the medical community. This system, passed into law by the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), will begin to take effect for physician reimbursement in 2019 but those payment adjustments will be determined by performance in various categories for services rendered in 2017. Regulations governing the application of this law have now been finalized and savvy radiology practices can begin to prepare to comply with the new system.
This is the second in our series of articles designed to help radiology practices prepare for MIPS. The first article, which covered Quality Performance, was published before the final rule and will be updated as soon as possible. Quality is the largest component of the MIPS score and will initially account for at least 60% of the total score. The Advancing Care Information (ACI) component initially will account for up to 25% of the total score. However, Eligible Clinicians (EC) for whom the objectives and measures of ACI are not applicable could see this category become 0%, with the 25% value being moved to the Quality Performance category, thereby increasing Quality Performance to 85% of the final score.
ACI Replaces Meaningful Use
Just as the Quality Performance category replaces the current Physician Quality Reporting System (PQRS), the ACI Performance category replaces the current Meaningful Use of Electronic Health Records (MU-EHR) program. However, the definition and focus of ACI has moved toward patient engagement, information exchange, and care coordination using Certified Electronic Health Records Technology (CEHRT) to promote better patient outcomes. Whereas the old MU-EHR program required 100% success in order to avoid a payment penalty, the ACI program will provide a score of up to 100 points that contributes to the overall MIPS Final Score.
The Meaningful Use program was measured and reported only at the individual provider level, but under MIPS the ACI reporting will be available for group reporting as well. This allows for one overall group performance score that will be applied to each individual EC in the group. For the 2017 performance year, either 2014 or 2015 CEHRT (or a combination of the two) will be allowed along with reporting of either Stage 2 or Stage 3 measures. ECs with 2014 technology for which certain ACI measures are not available may instead report the objectives and measures that correlate to Modified Stage 2, now called the "2017 ACI Transition Measures." For the 2018 performance year and beyond, 2015 CEHRT and Stage 3 measures will be required.
Exemptions from ACI
Radiologists might be able to avoid ACI reporting although there are some differences from the way this was handled under MU. There is no automatic exemption based on specialty as there was under MU. Instead, the ACI category will be re-weighted to a zero value if the radiologists fall under any one of the following circumstances:
- Hospital-based Eligible Clinicians - those who provide at least 75% of their services to Medicare patients using Place of Service Code 21 (Inpatient Hospital), 22 (Outpatient Hospital), or 23 (Emergency Department).
- Non-Patient Facing Eligible Clinicians - those who lack face-to-face patient interaction.
- In addition, radiologists may apply for ACI to be re-weighted to zero after the end of the performance year for the following circumstances:
- EC’s with insufficient internet connectivity available
- EC’s who lack of control over the availability of CEHRT
- EC’s with other extreme and uncontrollable circumstances
The exemption based on ‘lack of face-to-face patient interaction’ is one that contains some uncertainty about how it will be applied, even after CMS issued its final rule. The list of encounters that will be included for this determination has not yet been published by CMS, making it impossible for radiologists to know at this point if the exemption will be available to them or their groups. CMS has indicated that they will publish the list of patient-facing encounters prior to the January 1, 2017 start of the MIPS performance period.
- A non-patient facing EC is defined in the rule as one who bills 100 or fewer patient-facing encounters (including Medicare telehealth services) during the non-patient facing determination period (initially September 2015 to August 2016).
- Non-patient facing groups are defined as those where more than 75% of their ECs are deemed non-patient facing during the determination period.
In addition to these exemptions, certain practitioners such as Nurse Practitioners, Physician Assistants, Clinical Nurse Specialists, and Certified Registered Nurse Anesthetists will automatically be excluded from ACI for the first year of MIPS participation even though they are eligible for the overall MIPS program.
ACI Scoring
For those participating in ACI, points can be earned in the ACI Performance category as follows:
- Base score of 50 points
- Performance score of up to 90 points
- Bonus of 5 points for reporting to one or more public health or clinical data registries
- Bonus of 10 points for reporting improvement activities using CEHRT
Although it is possible to earn 155 points in this category, only 100 are needed to earn the full ACI Performance category value of 25 points toward the Final Score. The possibility to earn more points than are needed gives practices some latitude to add to their score in stronger areas in order to make up for points lost in weaker areas.
The Base Score
Earning points toward the base score in the ACI category will consist of answering and attesting to questions about the practice’s Certified Electronic Health Records Technology (CEHRT) system. ECs must simply provide the numerator/denominator or yes/no for each objective and measure. It is important to note that if the answer to Protect Patient Health Information is not ‘yes’ then a score of 0 will be assigned to the entire ACI Performance category.
There are either 4 measures under the standard ACI track, or 5 measures under the optional 2017 ACI Transition Measures track, across 4 categories (objectives) that will require reporting for the base score.
A Yes / No answer is required for:
Protect Patient Health Information - Conduct or review a security risk analysis addressing the security (including encryption) of data stored in CEHRT, implement security updates as necessary, and correct identified security deficiencies.
A Numerator / Denominator are required for:
Electronic Prescribing - At least one permissible prescription written by the EC is queried for a drug formulary and transmitted electronically using CEHRT.
Patient Electronic Access - Provide Patient Access: For at least one unique patient seen by the EC: (1) The patient* is provided timely access to view online, download, and transmit his or her health information; and (2) The EC ensures the patient’s health information is available for the patient* to access using any application of their choice that is configured to meet the EHR technical specifications.
Health Information Exchange:
* Or a patient-authorized representative.
For base score credit, at least one case must be reported for each of the available measures listed above.
The Performance Score
ECs may also choose to report measures using either the 2017 ACI Transition Measures track or the standard ACI measures for the performance score. Providers who report the 2017 Transition Measures will report up to 7 measures across 6 categories (objectives) where each measure is worth up to 10 or 20 points. The standard ACI measures track includes reporting up to 9 measures across 4 performance score categories where each measure is worth up to 10 points. There are 90 possible points in total for either track. Point allocation is determined on the basis of a provider’s numerator and denominator reporting for each measure as described in the table below.
For scoring purposes, CMS allows for rounding up to the next full point on any percentage that falls between two points. For example, a performance level of 92% on a 10-point measure would translate into 10 points (92% x 10 = 9.2 which would be rounded up to 10). The points for all measures are totaled to determine the ACI Performance Score.
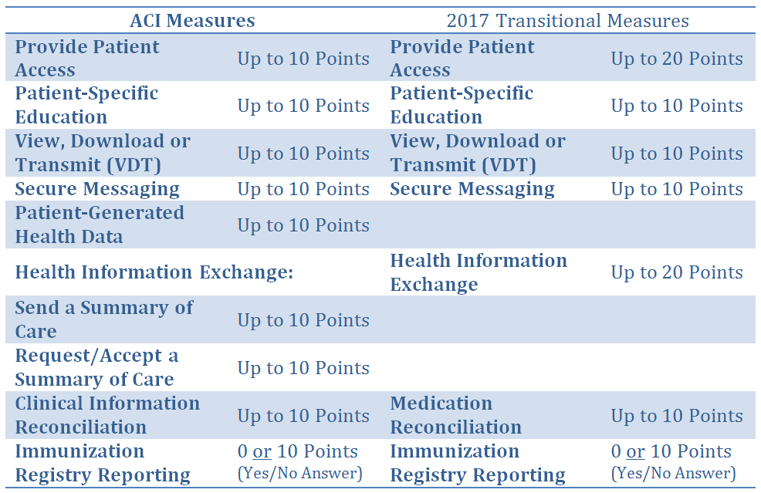
It is important to note that many of the individual measures do not apply to radiology, yet measure-specific exemptions that were available under MU are not available under ACI. In addition, most if not all of the bonus points that are available under ACI are also not applicable to radiologists. This might limit the ability of radiologists to participate in ACI.
Bonus Points
Up to 5 Bonus Points can be earned by reporting to any of the 4 optional registries directly from the CEHRT:
- Clinical Data Registry (such as the National Radiology Data Registry offered by the American College of Radiology)
- Public Health Registry
- Syndromic Surveillance Registry
- Electronic Case Reporting
The Immunization Registry is available for Performance Score points and and it cannot be used for claiming a bonus point.
Up to 10 Bonus Points can be earned by reporting specific Clinical Practice Improvement Activities (CPIA) that are defined under the CPIA performance category through the use of CEHRT.
MIPS Final Score
The ACI Base Score, Performance Score and Bonus Points (if any) are added together to determine the ACI Performance Score. Although it is possible to accumulate up to 155 points, only 100 points are needed to earn the full 25 points (or 25%) toward the Final Score under MIPS. A score of less than 100 points will contribute proportionately to the Final Score. For example, earning a total of 70 points in the ACI category would generate 17.5 points (70% x 25 = 17.5) toward the Final Score.
The ACI Performance category is worth 25% of the EC or group’s overall Final Score under MIPS. In addition to a contribution from ACI, the MIPS Final Score is made up of the Quality Performance category, which is worth 60%, and the Clinical Practice Improvement Activities (CPIA) category (worth 15%) of the total final score. If a radiologist can claim exclusion from the ACI Performance category, then the 25% allotted to that category will be redistributed to the Quality Performance category.
For 2017, the first reporting year of MIPS, the submission of even one measure from either the Quality or the CPIA category will allow an EC to avoid the 4% negative Medicare fee schedule adjustment in 2019. In addition, EC may also avoid the 4% payment adjustment by satisfying the ACI base score requirements. Partial participation in MIPS, defined as reporting some MIPS measures for any continuous 90-day period during 2017, will allow the EC to potentially qualify for a small positive payment adjustment based on the Final Score. Full participation in MIPS for any continuous 90-day period will allow ECs and groups to maximize their positive payment adjustments in 2019. Participation for a longer period, even the full year, will not necessarily improve the positive fee schedule adjustment, which will be based solely on the Final Score achieved. However, it will help to better prepare ECs and groups for future participation in MIPS by reviewing performance based on a full year of data.
Submitting Measures for ACI
Our first article included detailed information on the ways EC’s or groups can submit their measures data under the Quality Performance category. Those same options are available for submitting measures under the ACI Performance category, although it is not necessary to use the same method for the ACI Performance category as for the Quality Performance category. However, submissions for all MIPS categories must be done as either an individual or as a group.
How to Prepare for ACI Performance Reporting
Radiology practices that have been reporting under the Meaningful Use of EHR incentive program need to consider their continued participation under MIPS based on the requirements in the final rule. Those that have not previously reported will need to determine if they are now eligible under MIPS and, if so, whether they want to comply or possibly seek a hardship exemption from ACI. This will put more emphasis on their quality reporting.
In either case, it would be a good idea to review the available measures and determine which ones will allow the individual ECs or the group to achieve the best performance score. Review the reporting options, as well, to determine which method will be best suited to your practice.
Maria Calamaro serves as Product Director for Healthcare Administrative Partners and is the company’s subject matter expert for CMS quality programs. She has over 20 years of experience leading the product development and direction-setting for physician and hospital healthcare applications.
Subscribe to this blog to stay current with developments in this new program. Our next installments in this blog series will update the Quality Performance category based on the final rule, review the requirements of the Clinical Practice Improvement Activities, and provide a wrap-up of the overall MIPS program.
Related articles:
Transitioning Your Radiology Practice to MIPS: The Quality Component
Finalized MACRA Rules for 2017 Contain Some Good News for Radiologists



