Physicians’ Medicare reimbursement in the coming years will be impacted by their participation in CMS quality programs in 2014. Quality reporting programs such as PQRS, Meaningful Use and the new Value-Based Modification Program have allowed physicians to earn incentives for compliance with their requirements, but beginning in 2015 that carrot will become a stick. Medicare will apply penalties that reduce reimbursement for physicians that are eligible but do not participate in the programs. Payment reductions for 2015 have already been determined by participation in 2013, but there’s still an opportunity to take steps in 2014 to avoid a reduction in 2016 payments.
Physicians’ Medicare reimbursement in the coming years will be impacted by their participation in CMS quality programs in 2014. Quality reporting programs such as PQRS, Meaningful Use and the new Value-Based Modification Program have allowed physicians to earn incentives for compliance with their requirements, but beginning in 2015 that carrot will become a stick. Medicare will apply penalties that reduce reimbursement for physicians that are eligible but do not participate in the programs. Payment reductions for 2015 have already been determined by participation in 2013, but there’s still an opportunity to take steps in 2014 to avoid a reduction in 2016 payments.
Physician Quality Reporting System (PQRS)
The year 2014 is the final opportunity to report PQRS measures to earn an incentive payment of 0.5% of Medicare allowable amounts and avoid the PQRS penalty of 2.0% in 2016. The requirement has increased from three to nine measures, but even if you do not earn the incentive, you can avoid the 2016 Medicare reimbursement penalty.
You can report PQRS data as an individual or as part of a group. To report as a group (GPRO), you must practice with at least one other physician under the same taxpayer ID number. Individual reporting offers more options than group reporting as shown in this table:
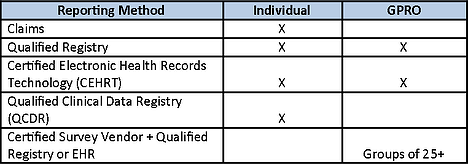
If you choose to report as a group, you must register with CMS by September 30, 2014. If a group registers and reports satisfactorily, all individual physicians in the group will be considered satisfactory PQRS reporters even if the individual does not have data reported based on individual services provided.
The Qualified Clinical Data Registry (QCDR) is a new reporting option for 2014. A QCDR is an entity approved by Medicare (such as a registry, certification board, collaborative, etc.) that collects medical and/or clinical data for the purpose of patient and disease tracking to foster improvement in the quality of care furnished to patients. Since the data measures collected are not limited to those defined in PQRS, a number of specialty societies have applied to have their registries become a QCDR. If approved, this option may offer specialists a preferable way to satisfy PQRS requirements through meaningful, relevant quality improvement activities.
In order to earn the incentive payment for 2014, the primary requirement under most methods is to report nine measures across three of the National Quality Strategy (NQS) domains for at least 50% of Medicare patients.
-
For Claims or Registry reporting, if fewer than nine measures are applicable, you only need to report those that apply. You will be subject to a Measures Applicability Validation (MAV) that verifies that all of the applicable measures have been reported.
-
If reporting by Registry, you can choose to report on a Measures Group instead of individual measures. This group must include a minimum of 20 patients with 11 or more covered by Medicare.
-
Reporting via Certified EHR Technology (CEHRT) does not require that 50% of the patients are Medicare beneficiaries. You can report only those measures for which you have Medicare patient data, provided there is at least one patient.
If you earn the 2014 PQRS incentive, you will automatically avoid the 2016 Medicare reimbursement penalty of 2.0%. Even if you do not earn this year’s incentive, you can avoid the 2016 penalty by reporting a minimum of three measures for 50% or more of your Medicare patients or by reporting fewer measures subject to review under the MAV. This alternative is only available if you report through claims or a registry.
Value-Based Modification Program (VM)
Participation in the PQRS program has additional Medicare reimbursement implications under the Value-Based Modification Program. This program was expanded in the 2014 Medicare fee schedule as mandated by the Affordable Care Act. Originally it applied only to large groups but ultimately it will include all Medicare providers. The VM payment adjustments are determined by the data gathered through PQRS.
-
Groups of 100 or more providers:
-
Payment modifications in 2015 are based on 2013 PQRS performance.
-
Payment modifications in 2016 are based on 2014 PQRS performance.
-
Performance modifications can be upward, neutral or downward.
-
2.0% penalty applies if no PQRS participation.
-
-
Groups of 10-99 providers:
-
Payment modifications in 2016 are based on 2014 PQRS performance.
-
Performance modifications can be neutral or upward.
-
2.0% penalty applies if no PQRS participation.
-
-
All providers:
-
Payment modifications in 2017 are based on PQRS performance in 2015.
-
Performance modifications can be upward, neutral or downward.
-
2017 penalty rates have not yet been defined.
-
Although based on PQRS data, the VM Medicare reimbursement adjustments are separate from any PQRS payment adjustments. The final regulations for application of the performance-based payment adjustments have not yet been issued.
Meaningful Use of Electronic Health Records (EHR)
Beginning in 2015, a 1.0% Medicare reimbursement reduction will be imposed on physicians who have not demonstrated meaningful use of an EHR in 2013 or 2014. To avoid a 2.0% reimbursement reduction in 2016, you must demonstrate meaningful use in 2014. This is also the last year you can begin participation and still earn an incentive payment.
Physicians who have completed two or more years of Stage 1 meaningful use must begin Stage 2 in 2014. Because all providers must upgrade or adopt newly-certified EHR software in 2014, all providers (regardless of when they began participating) are only required to demonstrate meaningful use for a 90-day reporting period in 2014. The reporting period is fixed to a calendar quarter. If 2014 is the first year you are demonstrating meaningful use, the 90-day reporting period must occur in the first 9 months of the year with attestation no later than October 1, 2014 to avoid the 2015 payment reduction.
For 2014, you must satisfy nine Clinical Quality Measures (CQM) from at least three NQS domains for the EHR meaningful use program. This aligns the CQM requirements under the EHR program with those of the PQRS program. Submission of this data under PQRS will satisfy the EHR meaningful use requirements as well, although there are some caveats in doing this:
-
Selected measures that have a zero in the numerator and denominator will not count for PQRS. They will count for meaningful use only.
-
PQRS requires a full calendar year of participation, while meaningful use in 2014 requires only 90 days of participation (aligned with a calendar quarter).
-
PQRS data must be submitted through a qualified registry to satisfy the meaningful use requirement of electronic reporting.
Physicians that meet certain hardship requirements that prevent participation in the program may apply for an exemption from the Medicare reimbursement penalty that begins in 2015 if they:
-
have been in practice for less than two years,
-
lack sufficient Internet access,
-
cannot participate due to extreme and uncontrollable circumstances,
-
do not have control over the availability of certified EHR technology at one or more practice locations, and the encounters at these locations constitute more than 50% of all patient encounters,
-
do not see patients face-to-face or via telemedicine and therefore can’t collect CQM data, or
-
use an EHR vendor that was unable to obtain 2014 certification or could not implement meaningful use due to 2014 EHR certification delays.
Exemptions will be granted year by year but may not continue for more than five years. An automatic exemption is available if you are enrolled in Medicare as an anesthesiologist, radiologist or pathologist without filing a manual application.
Failure to comply with the Medicare quality reporting provisions will be costly to physicians in the coming years. In 2016, the PQRS Medicare reimbursement penalty is 2.0%, the VBPM penalty is 2.0% and the EHR penalty is 2.0%. There’s no reason to believe that these penalties will not increase in the future. Even if you are exempt from meaningful use, the other penalties represent a potential 4% cut in Medicare reimbursement, which are already facing downward pressure from other factors. Avoiding these penalties means getting started now.